Comprehensive Epilepsy Center
What to Expect During Invasive Seizure Monitoring
INVASIVE SEIZURE MONITORING
After outpatient testing, your child may need additional evaluation to learn more about their seizures.
An inpatient hospital stay for invasive seizure monitoring is required for many patients. During invasive seizure monitoring, a neurosurgeon inserts electrodes into your child’s brain to learn about their seizures. This is done through Stereoelectroencephalography (sEEG) or Intracranial Grid Placement.
The goals of the invasive seizure monitoring are to:
- Learn the exact location of seizures in your child’s brain
- Determine if your child can be treated safely while targeting that area

SURGICAL PROCEDURES FOR INVASIVE SEIZURE MONITORING
sEEG
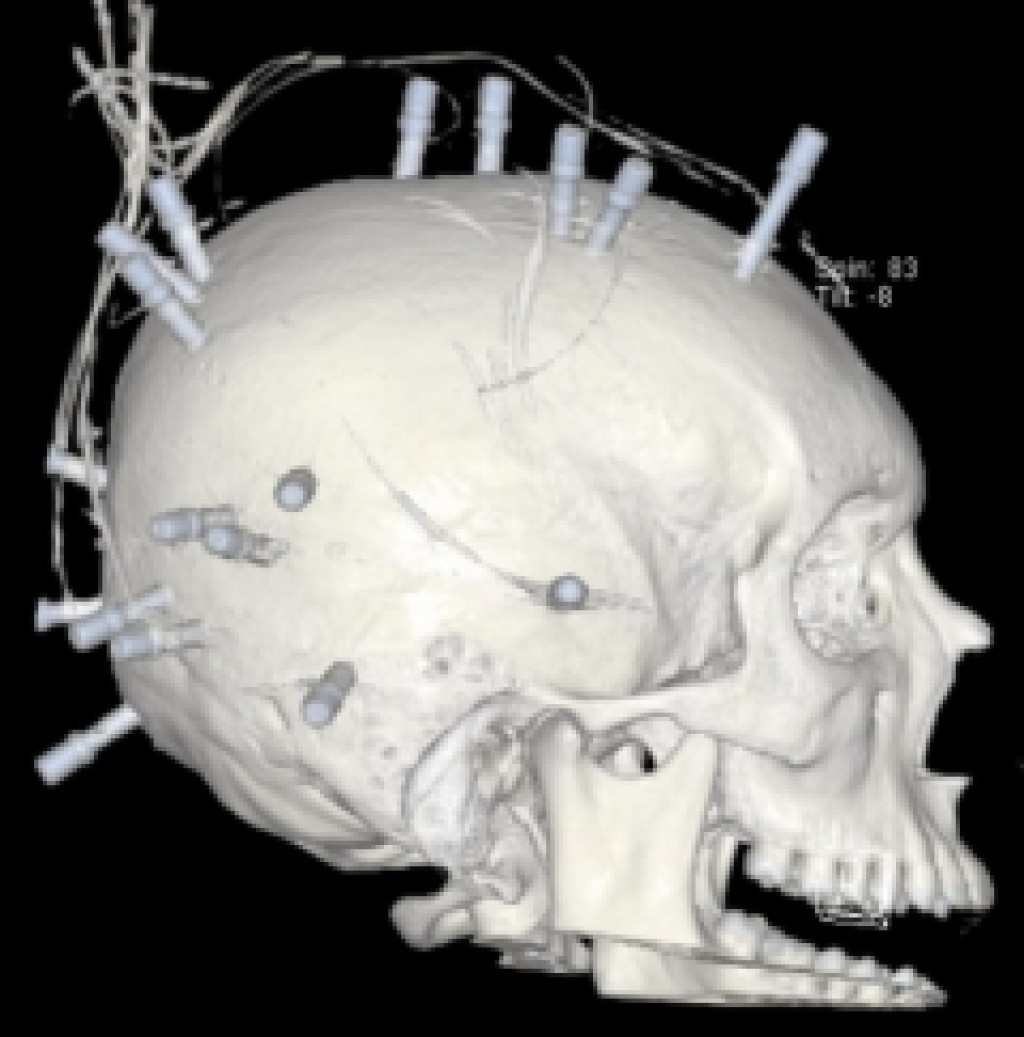
- About the Procedure: Small wires called intracranial electrodes are placed into brain tissue. A neurosurgeon drills small holes into the skull to implant the electrodes. An advanced robot helps guide and assist the surgeon to carefully place each electrode.
- Type of Incisions: Less invasive. Small holes about the size of a pencil eraser (4 mm) are drilled through the skull. Your child’s hair is not cut.
- Surgical Time: 3-6 hours
- Care Path After Surgery: Post-Anesthesia Care Unit (PACU), brain scan, Epilepsy Monitoring Unit (EMU)
- Appearance After Surgery: Parts of the electrodes will be visible outside of the scalp and your child’s head will be covered with a head wrap.
Intracranial Grid Placement
- About the Procedure: The skull is opened (craniotomy) to place a grid with electrodes directly onto the outer layer (cortex) of the brain.
- Type of Incisions: More invasive. Part of the skull is opened and replaced through a larger incision. Your child’s hair will be clipped along the incision line for this surgery.
- Surgical Time: 3-6 hours
- Care Path After Surgery: PACU, brain scan (CT or MRI), Neurosurgical Intensive Care Unit (Neuro ICU), EMU
- Appearance After Surgery: Your child has a head wrap in place with both electrodes and a drain coming from under the scalp.
ABOUT YOUR CHILD’S HOSPITAL STAY FOR INVASIVE SEIZURE MONITORING
Length of Stay

In order to monitor and record your child’s seizure activity, it is necessary for your child to stay in the hospital for a period of time. The length of this hospital stay could be as short as several days or as long as many weeks to gather all of the data needed to learn about your child’s seizures. Plan on staying at Texas Children’s Hospital for at least 2 weeks during Invasive Seizure Monitoring.
Managing Your Child’s Pain

It is common for children to have pain after this type of surgery. Your child will be given pain medication through an IV and by mouth. Your child will also receive antibiotics through an IV to help prevent infection while the electrodes are in place.
If your child is on a Ketogenic diet, it will be entered into your child’s electronic medical record and appropriate Keto-friendly pain medications will be given.
It’s Important to Stay in Bed
Your child will not be able to get out of bed to walk during their EMU stay. We know this is hard for your child and definitely not any fun. This is for your child’s safety.
Staying in bed means that your child cannot freely walk to a bathroom. A Texas Children’s team member will help your child use a bedpan when needed. In some cases, older children may be able to use a portable toilet or move to the bathroom with the assistance of a nurse.
Keeping Active in Bed
Staying in a bed for an extended time is difficult for anyone, but it’s especially hard for a child. Make sure to bring toys and activities from home that your child can enjoy while in bed. Our Child Life Team is available to work with you and your child to provide a wide range of activities such as art and music to provide support while your child is on bedrest. If your child enjoys dogs, we can place a request for a visit from one of our Golden Retriever hospital therapy dogs.
During Inpatient Seizure Monitoring, your child will not be able to receive physical or occupational therapy due to the bedrest restriction.
You should also bring activities that you enjoy. This is a difficult time for parents and caregivers as well. Remember to take walks and breaks throughout the day.
Encouraging Seizures
The Epilepsy Team observes and records your child’s seizures to get information on their location within your child’s brain. The Team may need to lower your child’s seizure threshold to pinpoint exact seizure locations. The Team is experienced at managing seizures and will have rescue medication ready to calm the seizures if needed. Slowly reducing seizure medication under the guidance of the Epilepsy Team and keeping your child awake for long periods without sleep are common ways to produce seizures. There is a nurse at the bedside at all times. Our EMU team is ready to support your child’s needs and you throughout this process.
Next Steps
After the seizure activity is recorded, the Neurosurgery and Epilepsy Teams hold a multidisciplinary meeting.
As a group, the Team may recommend a surgical intervention for your child. In some cases, additional electrodes are needed to gather more information about your child’s seizures.
The next surgery will include removal of electrodes and may include any of the following therapeutic procedures:
- Brain resection of the seizure focus
- Laser ablation of the seizure focus
- Corpus callosotomy
- Disconnection of the seizure focus through a hemispherectomy or quadrantotomy
- Brain stimulation including Responsive
- Neurostimulation (RNS), Vagus Nerve Stimulation (VNS), or Deep Brain Stimulation (DBS)

Your child will stay in the hospital to complete the recovery process. In rare cases, additional invasive electrodes are required after the therapeutic operation for a short time. The Neurosurgery and Epilepsy Teams will let you know when your child is ready to return home.
Please note that special circumstances may impact surgery scheduling and hospital guidelines. Your care team at Texas Children’s will update you if changes occur. Child Life Team provides music and art therapy.
LEAVING THE HOSPITAL
Your child will leave the hospital with the following items:
- A school note with activity restrictions.
- Wound care instructions – including how to wash the incisions 72 hours after surgery.
- Any prescribed epilepsy medications. Some patient are discharged home with antibiotics and steroids.
- A follow-up clinic appointment to see how your child is healing after surgery.
- Most patients will have a clinic visit 2 weeks after discharge.
-
Out-of-state/international patients may be able to arrange an earlier visit at the discretion of your surgeon.
Activity Restrictions

- Walking is the only physical activity allowed until your child is cleared by the Neurosurgery Team.
- No running, jumping, biking, skateboarding, weightlifting, swimming or other sports until your child is cleared.
- Returning to school and activity restrictions are decided on a case-by-case basis. Everyone recovers at their own pace.
When to call the Neurosurgery Team: 832-822-3950
Concerns related to surgery
- Any redness, swelling or drainage from your child’s incisions
- A fever of 101.5 or higher
- Headaches, vomiting, lethargy, abnormal eye movements, weakness in the arms or legs, or any other neurologic changes
When to call the Epilepsy Team: 832-822-5046
Concerns related to seizures
- Changes in seizure frequency after surgery
- Medication issues or questions
IMPORTANT CONTACT NUMBER
Epilepsy Surgery Nurse Coordinator 832-822-1100
- Patients and Visitors
- Preparing for Your Visit
- The Barbara Adams Family Resource Center
- Patients & Family Services Care Team
- Insurance, Financial & Billing Matters
- MyChart
- Cost Estimate
- Safety & Outcomes
- Caught You Caring!
- Health Professionals
- Refer a Patient
- Education
- Fellowships and Residencies
- Nursing
- Legislative Advocacy
- Medical Staff Credentialing
- Contact Us
