Topics
What is Sacrococcygeal Teratoma (SCT)?
A sacrococcygeal teratoma (SCT) is a tumor, or mass, that forms on the baby’s tailbone (coccyx) during fetal development.
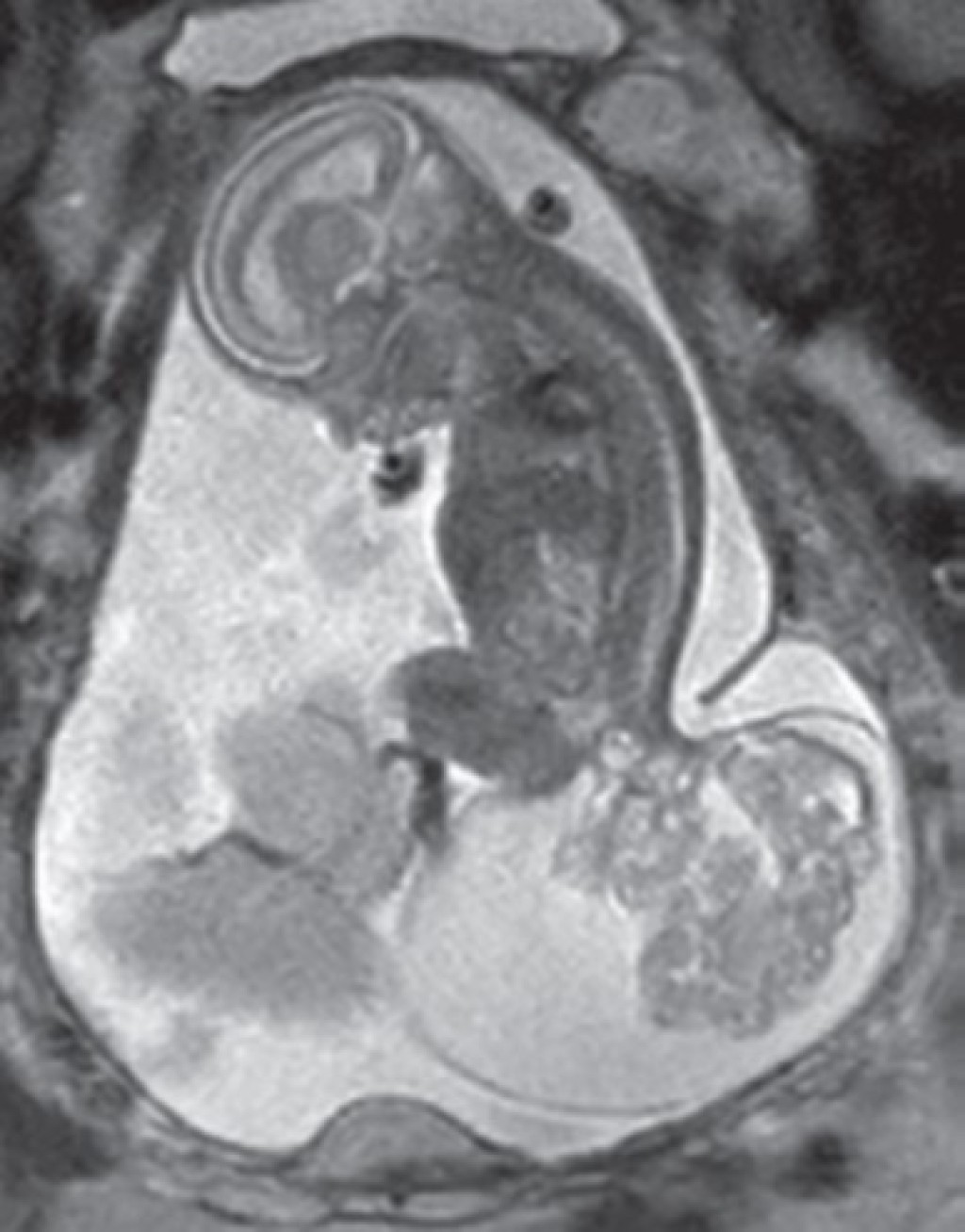
The tumor may be external, growing on the outside of the fetus, or internal, growing inside the body.
While sacrococcygeal teratomas diagnosed as infants or and prenatally are typically non-cancerous (benign), in some cases the tumor may grow quite large – even as large as the fetus – putting the baby and pregnancy at risk of serious complications. In rare cases they may also be cancerous (malignant).
Surgery is required to remove the tumor. After removal, the tumor is carefully evaluated under a microscope to determine if it is cancerous (malignant) or benign.

How does a sacrococcygeal teratoma affect my baby?
Sacrococcygeal tumors can develop large blood vessels that require high blood flow, causing the fetal heart to work harder to supply blood to the tumor and the rest of the body.
This can lead to an overproduction of amniotic fluid polyhydramnios and fluid accumulation and swelling in multiple areas of the baby’s body, a dangerous condition called hydrops which can lead to heart failure. Hydrops can develop rapidly and is often fatal for babies less than 30 weeks gestation.
In rare cases, when the tumor causes serious complications to the baby’s health, the mother may develop pre-eclampsia (high blood pressure), fluid retention and swelling that endangers her health, requiring immediate delivery. This is known as “maternal mirror syndrome,” where the mother’s health mirrors the health of her fetus.
Additional risks include:
- Preterm labor
- Bleeding from or rupture of the tumor
- Fetal urinary obstruction (hydronephrosis) caused by an internal SCT
- Need for a cesarean delivery, to avoid tumor rupture
Cause and Prevalence
Sacrococcygeal teratomas are rare, occurring in approximately 1 in 27,000 pregnancies. They are more common in female babies than males.
The cause of these tumors is unknown.
Types of Sacrococcygeal Teratomas
There are four types of sacrococcygeal teratomas, based on the tumor’s location and severity:
- Type I – completely outside the body
- Type II – primarily outside the body, with a small portion of the tumor inside the pelvic region
- Type III – a significant portion of the tumor is internal, extending into the baby’s abdomen
- Type IV – completely inside the body
The location of the tumor can affect diagnosis, treatment and prognosis, with the risk of malignancy highest in Type IV.
Diagnosis
In most cases, SCTs are diagnosed during pregnancy by ultrasound. If the mass is external it may be visible during a routine prenatal ultrasound.
More often, a specialized ultrasound is performed after a maternal blood test detects a high level of alpha-fetoprotein (AFP), which can indicate a tumor, or if the uterus is larger than normal, which may be caused by high levels of amniotic fluid or a large tumor.
If a sacrococcygeal teratoma is suspected or diagnosed, you may be referred to a fetal center with specialized expertise in these rare masses. At Texas Children’s Fetal Center, we arrange for you to visit as quickly as possible for a detailed assessment by a team of specialists experienced in the diagnosis and treatment of SCTs, including maternal-fetal medicine (MFM) physicians, fetal imaging experts, surgeons and fetal cardiologists.
Additional testing may include:
- High-resolution anatomy ultrasound to evaluate the mass
- Doppler ultrasound to measure blood flow to the tumor
- Ultra-fast MRI or low-dose CT for a more detailed view of the mass and fetal anatomy
- Fetal echocardiogram to assess heart function
- Amniocentesis and chromosomal analysis to screen for associated genetic abnormalities
Following this thorough evaluation, our specialists will meet with you about your results, answer any questions you have, and discuss your baby’s treatment needs.
Treatment During Pregnancy
Mother and baby will be closely monitored throughout pregnancy, with frequent ultrasounds and fetal echocardiograms to watch for signs of complications, including fluid accumulation, tumor size, blood flow patterns, and fetal growth rate.
In most cases, treatment of sacrococcygeal teratoma is surgery shortly after birth to remove the tumor (and the coccyx, to prevent recurrence).
However, in cases involving large tumors or tumors demanding high blood flow, life-threatening complications can occur during pregnancy that require fetal intervention. The goal is to reduce the demand for blood flow and prevent fetal heart failure.
If complications occur after 28 weeks’ gestation, the preferred fetal therapy is steroid administration to accelerate fetal lung development and early delivery, when necessary, with specialized care in a level IV neonatal intensive care unit (NICU). Prior to 28 weeks’ gestation, fetal surgery may be recommended to remove the mass, prevent fetal heart failure and prolong the pregnancy. The mass may be removed by open fetal surgery or radio-frequency ablation.
Open Fetal Surgery
In open fetal surgery, an incision similar to a C-section is made in the mother’s abdomen and the uterus is surgically opened, revealing the fetus. The tumor is removed or reduced in size while the fetus remains in the uterus. The site of the tumor removal is closed, the mother’s uterus and abdomen are closed, and the fetus continues to develop. The remainder of the pregnancy is closely monitored.
Open fetal surgery is performed in the hospital under general anesthesia; the fetus may also receive anesthesia.
All surgical procedures pose risks. The risks for open fetal surgery include harm to the fetus and premature labor. Talk with your healthcare team about the risks involved to help you make the most informed decision for you and your family.
A thorough evaluation should be conducted, including ultrasound, fetal echocardiogram and amniocentesis, to help determine if fetal surgery is an appropriate option. Only fetuses determined to have cardiac dysfunction prior to developing hydrops are considered candidates for open fetal surgery. Maternal “mirror syndrome” should also be ruled out before fetal surgery.
Delivery
Delivery should take place at a hospital with the expertise and resources required to care for babies with sacrococcygeal teratomas, including the highest level NICU. If the SCT is large, a cesarean delivery may be recommended.
Delivery and postnatal care should be carefully planned and coordinated across a team of maternal-fetal medicine, neonatal and pediatric specialists experienced in these high-risk births.
Our Fetal Center team works closely with pediatric experts from Texas Children’s Hospital, consistently ranked one of the best children’s hospitals in the nation, providing our patients seamless access to the critical care services and specialists their child may need after birth, including a level IV NICU.
For newborns with sacrococcygeal teratomas, this means no transfers during critical postnatal periods. It also means the pediatric specialists responsible for treating your child have been an integral part of their care team since before birth.
Postnatal Care Team
Babies with SCTs require regular follow-ups during the first few years of life to monitor for recurrence of the tumor.
Depending on your baby’s needs, his or her postnatal care team may include:
Why Texas Children’s Fetal Center?
- A single location for expert maternal, fetal and pediatric care. At Texas Children’s Hospital, you and your baby receive the specialized care required for the diagnosis and treatment of sacrococcygeal teratoma all in one location, for highly coordinated care and treatment planning, including immediate access to our level IV NICU.
- A skilled, experienced team with proven outcomes. We have a dedicated team of maternal-fetal medicine specialists, fetal imaging experts, neonatologists and surgeons, among many others, who work in concert to care for you and your baby, using proven protocols we’ve developed over the years. With their combined expertise and unified approach, this team offers the best possible care for these rare fetal tumors.
- We care for your child’s needs at every stage of life. Our comprehensive approach starts with your first prenatal visit and continues through delivery, postnatal care, and childhood, thanks to one of the nation’s leading teams of fetal and pediatric specialists.
Patient Stories

Fetal Surgery Removes Grapefruit-Sized Sacrococcygeal Teratoma
Nine years ago, at their 20-week ultrasound check, Keri and Chad McCartney were thrilled to learn their fifth and final child would be a girl. But that excitement quickly turned to fear.
Research and Clinical Trials
- Tumor volume to fetal weight ratio as an early prognostic classification for fetal sacrococcygeal teratoma.
Rodriguez MA, Cass DL, Lazar DA, Cassady CI, Moise KJ, Johnson A, Mushin OP, Hassan SF, Belleza-Bascon B, Olutoye OO. J Pediatr Surg. 2011 Jun;46(6):1182-5.
Volumes and Outcomes
In the News
- Fetal surgery removes grapefruit-sized mass (sacrococcygeal teratoma) from my unborn daughter
- Amos's story: Braving an early term sacrococcygeal teratoma diagnosis
- Meet the baby who was born twice
Videos
For more information or to schedule an appointment, call Texas Children’s Fetal Center at 832-822-2229 or 1-877-FetalRx (338-2579) toll-free.
Our phones are answered 24/7. Immediate appointments are often available.