Topics
Spina bifida is a birth defect that occurs when the spine doesn’t close properly during fetal development. It is a type of neural tube defect (NTD), abnormalities that affect the brain, spinal cord, or spine of a developing fetus.
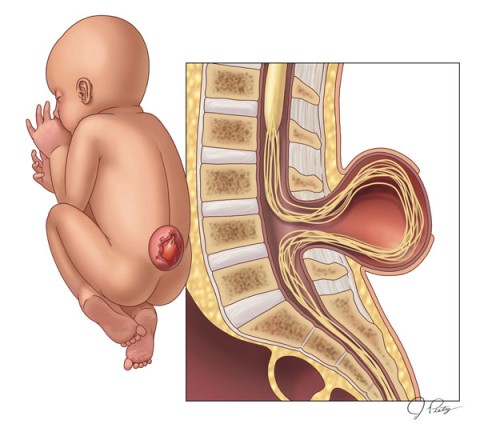
The most severe and common form of spina bifida is myelomeningocele. In this “open” neural tube defect, the spinal cord and surrounding nerves or other neural elements are exposed through an opening in the fetus’ back. This results in partial or complete paralysis of the parts of the baby’s body below the opening.
A neural tube defect may occur anywhere along the length of the spine but is commonly located along the lower back.
Myelomeningocele occurs in roughly 3 out of every 10,000 live births in the U.S. It is the most common birth defect of the central nervous system and the most common permanently disabling birth defect for which there is no known cure.
While surgery can repair the defect, spina bifida is a lifelong condition.
How does spina bifida affect my baby?
In patients with spina bifida and other neural tube defects, the spinal cord and nerves in the impacted area of the spine don’t function normally.
Common complications include:
- Problems with bowel and bladder function
- Paralysis, sensation loss, or weakness in the legs or feet
- Hydrocephalus, or fluid accumulation in the brain, requiring a shunt surgically implanted in the brain for drainage
- Developmental delay
Cause and Risk Factors
The exact cause of neural tube defects remains unknown. They occur during the first month of pregnancy.
Suspected risk factors include genetic issues, insufficient folic acid and other nutritional deficiencies in the mother, and environmental factors.
Women are at greater risk of having a child with a neural tube defect if they:
- Already have a child with spina bifida
- Have spina bifida themselves
- Have had a previous pregnancy affected by an NTD
Testing and Diagnosis
Spina bifida and other neural tube defects are typically diagnosed during a routine second trimester ultrasound. The most common symptom of myelomeningocele is a visible fluid-filled sac protruding through the skin, typically at the base of the spine, exposing an abnormally developed spinal cord.
Spina bifida may be suspected if a routine prenatal blood test, known as a maternal serum alpha fetoprotein (MSAFP) screening, detects high levels of alpha-fetoprotein in the mother’s blood, which can indicate the developing baby has spina bifida or other birth defects.
In less severe cases, a neural tube defect may not be detected until the baby is born.
If spina bifida is suspected or diagnosed during pregnancy, you may be referred to a fetal center for a comprehensive evaluation and specialized care.
At Texas Children’s Fetal Center, we arrange for you to visit as quickly as possible for a comprehensive assessment by a team of specialists experienced in diagnosing and treating these rare birth defects, including maternal-fetal medicine (MFM) physicians, fetal surgeons, pediatric neurosurgeons, fetal imaging experts, neonatologists, and pediatricians who specialize in the long-term care of babies with spina bifida.
Additional testing may include:
- High-resolution anatomy ultrasound to confirm the diagnosis and evaluate the defect
- Ultra-fast MRI for a more detailed view of fetal anatomy and function to assess the severity of the condition, including the effect on the developing fetal brain and any impact on fetal leg motion
- Fetal echocardiogram to evaluate your baby’s heart
- Amniocentesis and chromosomal analysis to identify chromosomal anomalies
Following this thorough evaluation, our specialists will meet with you about your results, answer any questions your family has, and discuss treatment options based on your baby’s defect and condition.
Treatment Options
Historically the treatment for babies with spina bifida has been surgery in the first few days after birth to close the defect. However, many babies develop hydrocephalus, or excess fluid in the brain, that needs to be drained through a shunt (hollow tube) surgically implanted in the baby’s brain for life. The child may face repeated surgeries to replace the shunt if it becomes infected or blocked over time.
In addition, the spinal cord and nerves protruding through the fetus’ back are exposed to amniotic fluid while in the uterus, which can cause progressive damage the longer the defect goes untreated.
To improve outcomes at birth, a landmark study was conducted on the fetal repair of myelomeningocele. This clinical trial, known as the Management of Myelomeningocele Study (MOMS), showed that surgery performed on the fetus to repair the defect leads to decreased rates of hydrocephalus, reducing or preventing the need for a shunt, and improved leg function compared to standard after-birth repair. The MOMS trial used an “open-hysterotomy” surgical approach, accessing and repairing the fetal spine through a 7-8 cm incision in the uterus.
Open Fetal Surgery
In 2011, Texas Children’s Fetal Center adopted open fetal surgery as our standard of care and began performing the procedure to treat spina bifida, as a continuation of the work done in the MOMS trial. As of June 2021, our physicians have completed 44 open fetal surgeries to treat bifida, with good outcomes. Risks of open fetal surgery include an increased incidence of preterm birth, the need for a cesarean section, and uterine rupture.
A First in Fetoscopic Fetal Surgery
In 2014, a multidisciplinary team at Texas Children’s performed an experimental fetoscopic closure of an NTD – the first in the nation. In this pioneering minimally invasive procedure, the spina bifida repair is performed through two tiny (4 mm) incisions in the uterus, reducing the risks to mother and fetus associated with a large uterine incision.
Fetoscopic fetal surgery to repair spina bifida can lead to longer gestation, improved outcomes, lower rates of hydrocephalus, decreased need for shunts and improved leg function compared to after-birth repair. It may also preserve the mother’s ability to deliver vaginally following the initial repair and for future pregnancies.
As of November 2025, our fetal center physicians have completed more than 220 fetoscopic repairs, more than any other fetal center in the United States.
Fetoscopic Repair – About the Procedure
Fetoscopic repair surgery is typically performed between 19 and 26 weeks of gestation.
During the procedure, the mother’s abdomen is opened and two 4-millimeter incisions are made in the uterus. Guided by ultrasound, the surgeon accesses the fetal tissue and closes the defect, protecting the spinal column and nerves from infection and injury for the remainder of gestation. Carbon dioxide gas is inserted into the uterus to improve visualization of the fetus.
Following fetal surgery, the mother will stay in the hospital 4 to 7 days. Mother and baby will be closely monitored for the remainder of the pregnancy.
Fetoscopic repair patients that meet a defined criteria of post-surgery clinical stability as well having the necessary maternal, neonatal, and neurosurgical care team and facility resources near home may be released back to their referring provider a few weeks after surgery for ongoing care until delivery. Patients that undergo open repair are generally advised and expected to remain under the care of our Fetal Center team from the time of surgery until their delivery.

Benefits of Fetoscopic Repair
This minimally invasive approach offers benefits over both open fetal surgery and surgical repair after birth.
Benefits compared to open fetal procedure include:
- Opportunity for vaginal delivery, unlike open fetal surgery which requires a cesarean delivery
- Reduced risk of uterine rupture or rupture along the surgical incision, through the use of two very small incisions
- Avoid the risk of premature birth and increase gestation time; the average age at delivery with fetoscopic surgery is 37-38 weeks
Benefits compared to surgical repair after birth include:
- Prevent or reduce the need for a brain shunt, and the potential need for repeated shunt surgeries, by decreasing the risk of hydrocephalus
- Preserve nerve function and potentially the child’s ability to walk by protecting the spinal nerves from exposure
Is my baby a candidate for fetal intervention?
A comprehensive evaluation of your pregnancy is essential to determining whether fetal surgery for myelomeningocele is an appropriate intervention. Patients who meet all inclusion criteria and none of the exclusion criteria of the MOMS trial are considered candidates for prenatal spina bifida repair.
If you and your baby are both candidates for fetal surgery, you will meet with our fetal specialists to discuss the risks and benefits of the procedure in detail, to help you and your family decide the best treatment approach for you.
Our patients are counseled on both open-hysterotomy repair and fetoscopic repair. Open hysterotomy is generally considered the clinical standard of care for prenatal repair. However, given the experience and outcomes in our Fetal Center, fetoscopic repair is also considered standard of care in our institution.
Inclusion and Exclusion Criteria
Guidelines for both fetoscopic and open procedures are based on the criteria set forth by the MOMS trial.†
Inclusion Criteria
- Myelomeningocele (MMC) at T1 through S1 with hindbrain herniation, level of MMC confirmed by ultrasound and hindbrain herniation confirmed by MRI
- Maternal age greater than or equal to 18 years
- Gestational age 19 0/7 weeks to 25 6/7 weeks at the time of prenatal surgery
- Normal karyotype or FISH
- Normal fetal echocardiogram
- Singleton pregnancy
- Willing to remain close to Texas Children's Hospital
Exclusion Criteria
- Significant fetal anomaly not related to MMC
- Kyphosis in fetus of greater than 30 degrees
- History of incompetent cervix, cervix less than 20mm or presence of a cerclage
- Morbid obesity as defined as a BMI of greater than 40
- Maternal-fetal Rh isoimmunization, Kell sensitization or a history of neonatal alloimmune thrombocytopenia
- Maternal HIV, Hepatitis B, Hepatitis C due to increased risk of transmission to the fetus during maternal-fetal surgery
- Uterine anomaly such as large or multiple uterine fibroids or mullerian duct abnormality
- Maternal medical condition which is a contraindication to abdominal surgery or general anesthesia
- No support person to stay with mother at Ronald McDonald House
- Patient does not meet psychosocial criteria as determined by the social worker evaluation
- Previous hysterotomy in the active segment of the uterus either from previous classical cesarean section, uterine anomaly such as an arcuate or bicornuate
†Adzick, S., Thom, E., Spong, C., Brock, J., Burrows, P., Johnson, M., Farmer, D. (2011). A randomized trial of prenatal versus postnatal repair of myelomeningocele. New England Journal of Medicine, 364, 993-1004.
Referrals
We welcome all referrals. Candidates are carefully evaluated and accepted for maternal-fetal surgery on a case-by-case basis. Please contact us at 832-822-2229 if you are a physician and would like to discuss the eligibility of your patient for the fetoscopic procedure.
Medical algorithm of fetal myelomeningocele neural tube defect (Revised 9/2015)
Delivery
For the best possible outcomes, babies with spina bifida should be delivered at a hospital with the specialized expertise and resources required to treat neural tube defects, including the highest level of neonatal intensive care (NICU), if needed. Texas Children’s Hospital is home to the first NICU to be designated by the Texas Department of State Health Services (DSHS) as a level IV NICU, the highest level of care available for premature and critically ill newborns.
In addition, our fetal center specialists work closely with Texas Children’s Spina Bifida Program to coordinate your baby’s care from prenatal diagnosis through delivery, avoiding the need to transfer your newborn during the critical postnatal period.
This collaborative approach means the pediatric experts who will care for your child at birth have been an integral part of the care team every step of the way.
Treatment After Birth
Texas Children’s Spina Bifida Program
Exceptional postnatal care for spina bifida patients at Texas Children’s Hospital
A unique and distinct advantage for all mothers delivering at Texas Children’s Pavilion for Women is our location inside of one of the largest and most renowned children’s hospitals in the world. For babies with fetal conditions such as spina bifida, this means no transfers during critical postnatal periods. It also means that the pediatric experts responsible for treating a child after birth have been an important part of the care team prior to birth as well.
Texas Children’s provides a comprehensive neurodevelopmental and postnatal follow-up program for patients born with spina bifida led by Dr. Jonathan Castillo Porter, developmental pediatrician. For more than 30 years, our multidisciplinary program has brought world-renowned experts from several specialty services together to provide the best possible care for spina bifida patients such as neurosurgery, urology, developmental pediatrics, physical medicine and rehabilitation, orthopedics, orthotics, physical therapy, nutrition, child-life and more.
The program offers neurodevelopmental assessments and complex care management to help patients with frequent spina bifida comorbidities such as hydrocephalus, developmental and behavioral concerns, tethered cord syndrome, scoliosis, neurogenic bladder, neurogenic bowel and impaired motor ability.
Patients are followed from birth until 18 years of age in the Spina Bifida Program. Patients under 1 year of age typically are seen every three months. Patients 2-4 years old typically are seen every four to six months. School-aged patients typically are seen once a year. Patients over the age of 18 graduate to a transition medicine clinic with Baylor College of Medicine. The Texas Children’s Spina Bifida Program offers a clinic that focuses on transitional needs so patients are well equipped to move on to a physician focused on adult care.
For more information about Texas Children’s Spina Bifida Program, please call 832-822-4308.
Why Texas Children’s Fetal Center?
- A single location for expert maternal, fetal and pediatric care. At Texas Children’s Hospital, you and your baby receive the specialized care required for the diagnosis and treatment of spina bifida all in one location, avoiding the need to transport your critically ill newborn.
- A skilled, experienced team with proven outcomes. We have a dedicated team of maternal-fetal medicine specialists, fetal surgeons, neonatologists, fetal imaging experts, pediatric neurosurgeons, pediatric urologists, and others who work in concert to care for you and your baby every step of the way, using proven protocols we’ve developed over the years. With their combined expertise and unified approach, this remarkable team offers the best possible care for babies with spina bifida.
- We care for your child’s needs at every stage of life. Our comprehensive approach starts with your first prenatal visit for spina bifida and continues throughout your child’s delivery, postnatal care, childhood and adolescence, thanks to one of the nation’s leading teams of fetal and pediatrics specialists for the treatment of rare neural tube defects.
Volumes & Outcomes
As of January 2019, Texas Children’s Fetal Center has completed 100 prenatal neural tube defect (NTD) surgical repair procedures to treat spina bifida, more than half of which were fetoscopic in-utero repairs.
Research and Clinical Trials
Texas Children’s Fetal Center participates in research and clinical trials to offer families the broadest number of options for the treatment of neural tube defects.
Learn more about these trials:
Spina Bifida in the News
- 1-year-old who had surgery inside womb to correct spina bifida now standing on 2 feet (Goodd Morning America - 06/28/19)
- After Surgery in the Womb, a Baby Kicks Up Hope – (The New York Times - 01/15/2018)
- Lights, Camera and, Yes, Music: Reporting From the Operating Room as Doctors Perform Fetal Surgery – (The New York Times - 10/24/17)
- To Mend a Birth Defect, Surgeons Operate on the Patient Within the Patient – (The New York Times - 10/23/2017)
- Everett’s update: Flourishing after fetoscopic surgery (Pavilion for Women's Blog - 1/31/19)
- Scars unite new mom, son (CNN - 3/8/17)
- Bellamy's story: Fetoscopic surgery for spina bifida (Pavilion for Women's Blog - 11/17/18)
- Our spina bifida and fetal surgery story: Part 1 (Pavilion for Women's Blog - 7/17/17)
- Our spina bifida and fetal surgery story: Part 2 (Pavilion for Women's Blog - 7/17/18)
- My living champion: Fetoscopic surgery to repair spina bifida (Pavilion for Women's Blog - 6/17/17)
- From Georgia to Houston: Our spina bifida fetal surgery journey (Pavilion for Women's Blog - 6/17/17)
- What a difference a year can make (Pavilion for Women's Blog - 2/8/17)
- Giving our son the best chance with fetal surgery for spina bifida (Pavilion for Women's Blog - 8/17/16)
- My son’s first surgery for spina bifida (Pavilion for Women's Blog - 8/3/16)
Patient Stories

Emerson's story: When life gives you lemons
When life gives you lemons, make lemonade. I imagine nearly everyone has heard this old saying before. In other words, find the positive in a negative situation. In our case, we’ve been doing our best to “make lemonade” ever since finding out our daughter, Emerson Grace.

God's answered prayer: Olivia
At their 18-week ultrasound, expecting parents Ashley and Jason learned their daughter, Olivia, had signs of spina bifida. Learn more about their journey at Texas Children’s Fetal Center and how the Fetal Team saved their daughter’s life with this innovative fetal surgery.

Canezaro Family first to undergo successful two-port fetoscopic spina bifida repair in U.S.
When Althea Canezaro found out she was pregnant, she was thrilled to give her son, Blaine, a sibling. But, her 22-week ultrasound revealed something she didn’t expect - spina bifida.

Less Invasive Approach to Fetal Spina Bifida Repair
Julia Wallace vividly remembers the moment a routine ultrasound revealed her unborn daughter had myelomeningocele, a type of spina bifida.

The Future of Healing for Neural Tube Defects
Like most first-time parents, Johnna and Adam Kerres of Rock Island, Illinois, were excited to mark every milestone of their pregnancy. Until, that is, an ultrasound at 18 weeks revealed their baby boy Everett had spina bifida.

Surgery Before Birth Changes Abdiel’s Life
Texas Children’s Hospital fetal surgery to repair spina bifida birth defect saves child from paralysis, brain damage and other life-altering complications.
For more information or to schedule an appointment,
call Texas Children’s Fetal Center at 832-822-2229 or 1-877-FetalRx (338-2579) toll-free.
Our phones are answered 24/7. Immediate appointments are often available.