Le Fort 2 osteotomy with simultaneous zygomatic repositioning (LF2ZR) is a surgery that brings the central part of the face (nose and upper jaw) forward and down and the cheekbones up. It is also known as “segmental subcranial distraction advancement”. LF2ZR is a type of Le Fort osteotomy that uses the power of distraction osteogenesis for the bigger movement of the central face, and small plates and screws to achieve the smaller cheek bone movement. In North Austin we use this powerful surgery in the treatment of Apert syndrome and Pfeiffer syndrome, but have also experience in using it to treat other midface conditions such as in Achondroplasia.

One of our surgeons was the first to describe this procedure and has the most experience in performing it safely.
- We use a technique known as “distraction osteogenesis” to move the Le Fort 2 bone forward. Since the cheekbones do not need to move as much but in a different direction, we reposition those separately and secure them with small plates and screws.
- Distraction osteogenesis allows us to move the Le Fort 2 bone forward greater distances to lengthen the nose and middle of the face and bring the upper teeth forward and down.
- The cheekbones in Apert and Pfeiffer syndrome only need to move forward and up a small distance, so we do this during the same surgery but hold them in place using titanium plates and screws. Titanium is a metal that our bodies accept easily. We often use titanium plates to fix broken bones after trauma. The two small plates we use in LF2ZR are so thin and small that they do not set off airport alarms and do not need to be removed.
- LF2ZR is a full-day operation
- Our surgeons start by performing a Le Fort 3 osteotomy through a coronal incision to prepare the face for movement after surgery. (Figures A and B below)
- They next separate the cheekbones from the Le Fort 3 segment, leaving a Le Fort 2 segment. The cheek bones are then moved forward and up ¼ “ and held in the new position with one thin titanium plate and screws on each side. (Figures C to F below)
- This cheekbone movement support the eye position and give better cheek protection.
- The surgeon then wires a custom splint made by our orthodontist to the upper teeth to move the Le Fort 2 segment after surgery. (Figure G below)
- At the end of the surgery, your surgeon attaches a “halo” distractor to your child’s skull and it attaches to the custom splint. In some cases we will apply the distractor a day or two after the LF2ZR surgery during a brief operation. (Figure H below)
- Your child will remain in the ICU under sedation for the first 2-3 days after surgery. If they do not have a tracheostomy, we will usually keep their breathing tube in place until their swelling starts to go down
- While your child is recovering at home, a parent or other caregiver turns little screw posts on the device twice a day for 2 to 3 weeks. This brings the upper jaw forward and down at a rate of 1-2 mm a day.
- After turning is complete and once everything is in the right place, the distractor stays on for 6 to 8 more weeks. This helps the bone heal in its new position. New bone will grow and fill in the gaps and stabilize the face in its new position.
- After healing phase is over, we will remove the distractor in a short operation. Your child does not need to stay the night and goes home after the surgery.

- The average age of patients who our surgeons have treated with Le Fort 3 surgery are 8 years old. We usually recommend waiting until at least 7 years of age before having the surgery, but the surgery can be done at any time after that with the same results.
- Before surgery, all children undergoing midface surgery will have their front teeth far behind their bottom teeth. After LF2ZR advancement we will intentionally over-correct this difference so that the front teeth are ¼ to ½ inches in front of the lower teeth. We do this to plan for continued growth of the lower jaw to catch up.
- Almost all patients who have a LF2ZR advancement when they are younger will still require corrective orthognathic (jaw) surgery to finalize their bite after orthodontic treatment.
- Is a blood transfusion needed during the surgery?
- Yes, a blood transfusion is required to keep your child’s blood levels safe during the surgery. We will draw blood work before surgery to prepare and you will sign a separate consent form.
- What should I expect during the time in hospital?
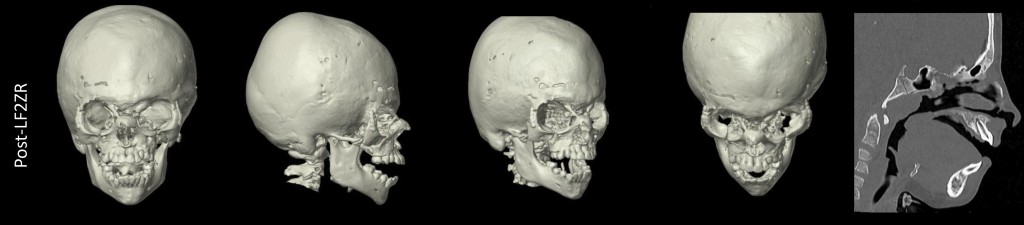
- After surgery your child will be taken to the CT scanner for a post-surgery image, and then taken to the Pediatric Intensive Care Unit (PICU). We will reunite you with your child as soon as possible after the PICU team has assumed care.
- It can be emotional to see your child for the first time in the PICU since they will have the distraction device in place and a number of tubes to help with giving fluids and nutrition. They will be kept very sedated for 24 hours to keep them comfortable. Swelling of the face will be the most 24 hours after surgery and will last 2-3 days before the swelling quickly goes down.
- Your child will be transferred to the hospital inpatient ward after 2-3 days in the PICU. Total length of time in the hospital is 5 to 7 days. You will be able to stay with your child throughout the hospital say. We recommend you take time to rest outside of the hospital while your child is in the PICU, or alternate with another caregiver. It is important you are not sleep-deprived when they go to the ward since you will be more involved in their care after that and will start to learn to turn the distraction devices.
- How do you control my child’s pain after the procedure?
- During the time in the PICU, your child will receive pain medicine through their intravenous lines and will be kept sedated for their comfort. After 24 hours they will be allowed to be more awake and we will start to transition their pain medications to acetaminophen (Tylenol), ibuprofen, and a prescription pain medicine called oxycodone.
- These are the three medications your child will continue after they are discharged from hospital, but the oxycodone is only needed for a few days. Acetaminophen and ibuprofen is given as needed during the turning phase of distraction, but is rarely needed during the healing phase.
- How difficult is it to turn the devices?
- Parents have reported that they found turning the devices a lot easier than they had anticipated. The small screwdrivers used to turn the device have arrows to show the director of turning and are easy use after a few tries. We will provide you with a small calendar to record each turn that is done in the morning and again in the evening.
- Does turning the device hurt my child?
- Your child should not feel pain when you turn the devices. The devices move the face very slowly at a rate of 1 to 2 mm per day. Early in the turning phase the screwdrivers are easy to turn, and your child usually does not feel any movement. Towards the end of the 2-3 week turning phase the muscles can start to stretch, and your child may feel an ache after turning that is like the feeling after having orthodontic braces adjusted. This is usually managed with over-the-counter acetaminophen (Tylenol) and ibuprofen.
- What will my child feel like during the turning phase?
- Although families usually mentally prepare themselves for the surgery and hospital stay, we will also help you prepare for the turning phase. Even though the turning of the devices does not cause pain, your child’s face is slowly and steadily moving forward over weeks, and therefore it does not have time to fully heal until the turning phase is complete.
- Families who have undergone Le Fort 3 procedure describe the turning phase as tiring. Your child will need your emotional support during this phase and encouragement that what they are feeling is temporary and that they will feel better after the turning is over. We have child life and child psychology teams available to you during this time if needed. Turning of the devices often causes drooling and extra saliva production. This stops quickly after the healing phase begins.
- If we don’t live within easy driving distance from the hospital, how long will we need to stay in Austin?
- After your child is discharged from the hospital, we will need to see them in our clinic once a week during the entire turning phase. During these visits we will take an x-ray to track the movement of your child’s face and the change in their airway shadow.
- Your surgeon may need to make some minor adjustments to the device during this period. These are done in clinic and do not cause any pain.
- We do not need to see your child in clinic during the healing phase after turning is complete but will keep in touch through messaging and video visits.
- Families who live out-of-state will usually arrange to have temporary lodging in Austin for 3 to 4 weeks to complete the surgery and turning phase. At that point your child can return home either on the plane or by car.
- What will my child feel like during the 6 to 8 week healing phase?
- During the healing phase at home, your child will want return to many of their pre-surgery activities. Since the halo device is no longer being turned, their bones start to heal quickly, and their face quickly starts to feel more normal to them. They just need to avoid activities that would put their halo device at risk, such as ball games, energetic play, or running. If your child was experiencing drooling during the turning phase, it usually quickly stops during the healing phase.



Every child with Apert syndrome is unique, but there are some common changes in the face of children undergoing LF2ZR. The surgery lengthens the nose and makes the bridge of the nose more prominent. It rounds out the center of the face, creates more cheek bone structure and usually helps with closure of the lips. The changes in the face gradually soften and become more smooth over time as the bones of the face heal and remodel to adjust to their new position.
- Our Team Child Psychologist created a checklist that you may find helpful to prepare your child emotionally, mentally and physically for a large facial reconstructive surgery.
- If you would like for your child to meet with our Child Psychologist before or after a surgery, please let us know and we can arrange a consult.