Topics
NRI researchers develop a rat model of Rett Syndrome
Rett syndrome (RTT) is a neurodevelopmental disorder that affects the X chromosome and is almost exclusively seen in young girls. Boys with this condition do not survive since they do not have a second normal copy of the X chromosome to compensate for this defect.
Girls diagnosed with RTT develop normally early on, but soon they start to show signs of regression. They quickly lose most of their acquired psychomotor skills such as purposeful use of their hands, distinctive hand movements and walking. This is accompanied by seizures, intellectual and cognitive disabilities including autism, schizophrenia, obsessive-compulsive disorder, attention-deficit hyperactivity disorder and many other cognitive problems.
Mutations in a master regulator protein, methyl-CpG-binding protein (MeCP2), are known to cause RTT. In the past few decades, mouse models with defects in MeCP2 function have greatly advanced our understanding of this disorder. But their critical drawback is they do not mimic some of the most useful and relevant clinical features of the human condition.
Thus, it is becoming increasingly apparent that reliance on a single rodent species to develop RTT drugs limits our ability to measure crucial molecular, biochemical and behavioral outcomes, and in the end, may not lead to the most effective treatments. Lack of rigorous evaluations in multiple animal species and use of suboptimal animal models at the preclinical stages are among the most common reasons why drugs developed for neurobehavioral disorders routinely fail during clinical trials.
To address these issues, a team of researchers at the Neurological Research Institute (NRI) at Texas Children’s Hospital led by Dr. Rodney Samaco, assistant professor at Baylor College of Medicine, characterized a novel genetic rat model of RTT that closely mimics many behavioral and molecular features of RTT patients. This study was published last week in the Human Molecular Genetics journal, with Dr. Surabi Veeraragavan, an instructor at Baylor College of Medicine, as the lead author.
After confirming the rat model of RTT was missing the MeCP2 protein, the researchers set out to test the behavior of the animals, focusing on female rats. Among the tests they conducted were two behavioral features in RTT rats that have not been previously observed in RTT mice.
First, the team measured psychomotor regression, performed a de-shelling assay. Typically, normal and mutant rats take about 100 seconds to de-shell a handful of seeds. With time, normal rats learn to do it much faster, while RTT rats take even longer, indicating a regression in their acquired psychomotor skills. This is the first time that ‘loss of an acquired skill over time’, an important clinical indication used to diagnose a RTT patient, has been demonstrated in a rodent model of RTT.
Second, because rats are smarter with advanced social and cognitive behaviors than mice, the researchers asked whether the RTT rats showed problems in complex social interactions. Typically, juvenile rats are constantly roughhousing, just like children, showing a degree of ‘play’ that is far more complex than in young mice of the same age. Interestingly, the researchers found that young female rats lacking MeCP2 protein engaged less in specific aspects of play when paired with a normal rat.
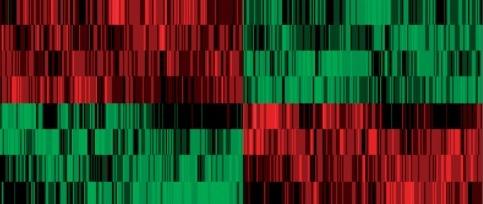
Beyond these behavioral features, Samaco and his team also examined gene expression patterns in the brains of RTT rats. They came across a very insightful finding by first comparing the RTT rat data to existing RTT mouse data, and then testing gene expression in archived brain tissue from RTT patients. While rats may better reflect the timing and onset of behavioral problems in RTT, using rats and mice together allows researchers to accurately predict the molecular and biochemical changes in the brains of RTT patients.
To conclude, Samaco and his team believe this new rat model is an important addition to the toolbox of RTT researchers that will shape the landscape of future preclinical studies and may expedite the discovery of an effective therapy.
Reference:
Veeraragavan S et al., Loss of MeCP2 in the rat models regression, impaired sociability and transcriptional deficits of Rett syndrome . Hum Mol Genet. 2016 Jun 30. pii: ddw178.




