Topics
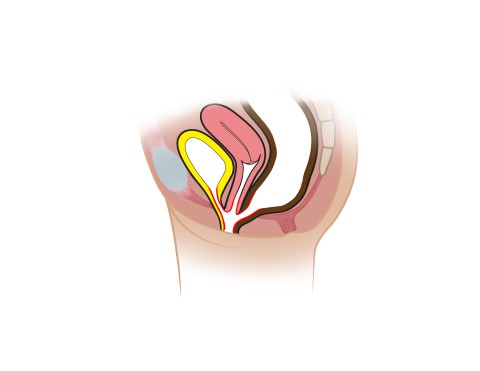
A cloacal malformation, or cloaca, is a rare condition that occurs in 1 in 25,000 girls. It is a severe form of anorectal malformation that occurs early in fetal development, in which the rectum, vaginal tract and urinary tract fail to separate. These structures merge into one common channel called a cloaca. The length of the common channel can vary in length and will affect how the malformation is prepared.
Type
Cloacal malformations are usually described as either “short” (less than 3 cm) or “long” (greater than 3 cm) common channel. The length of the common channel will determine how the surgery is performed.
Diagnosis
Cloacas can be diagnosed before birth on ultrasound; there may be abnormalities in the urinary structures or a cystic mass in the pelvic. Most of the time a cloaca is diagnosed after birth when a single opening is seen on the perineum.
When your child is several months old, an exam under anesthesia with a cloacagram will be performed to map out your child’s anatomy. This will help determine how the cloaca will be repaired.
Treatment
All cloacas undergo colostomy creation shortly after birth. Following the exam under anesthesia, the team will plan the approach for your child’s cloacal repair depending on the length of the common channel and urethra.
Most cloacas with common channel less than 3 cm can be approached by a similar approach to a PSARP, called a posterior saggital anorectal vaginal urethral plasty (PSARVUP). The pediatric surgery team will separate the rectum from the common channel and place it within the sphincter complex. The urologists and gynecologists will use the length of the urethra to determine if the urethra and vagina are reconstructed by either a total urogenital mobilization (TUMS) or total urogenital separation. For longer common channels, the surgeons may need to approach the repair through the abdomen.
Some patients may require vaginal reconstruction if the vagina cannot reach the perineum. The team may use part of the bowel (intestines) to help with the replacement.