Fetoscopic Repair of Spina Bifida


Topics
Fetal surgery to repair spina bifida can improve infant outcomes compared to after-birth repair.
There are two options for prenatal repair: open fetal surgery and fetoscopic fetal surgery, a minimally invasive approach that reduces the risks associated with a large uterine incision.
While surgery can repair the birth defect, spina bifida is a lifelong condition.
Spina bifida is a birth defect that occurs when the spine doesn’t close properly during fetal development.
The most severe and common form of spina bifida is myelomeningocele, a condition in which the spinal cord and surrounding nerves are exposed through an opening in the fetus’ back. Also known as an “open” neural tube defect (NTD), the result is partial or complete paralysis of the parts of the body below the opening. In addition, spina bifida is usually associated with the accumulation of cerebrospinal fluid in the brain.
Historically the standard of care was closure of the defect during the first few days of an infant’s life. However, many babies develop hydrocephalus (severe fluid in the brain), requiring brain shunts (drains) for life.
A landmark clinical trial known as the Management of Myelomeningocele Study (MOMS) demonstrated in 2011 that fetal surgery to repair the defect can improve infant outcomes compared to after-birth repair. The MOMS trial used an “open-hysterotomy” approach (incision across the uterus).
Benefits of prenatal repair include:
In 2011, Texas Children Fetal Center adopted open fetal surgery as our standard of care, the approach used in the historic MOMS study. We were one of the first centers to perform the procedure to treat spina bifida.
In this open-hysterotomy surgical approach, the defect in the fetal spine is accessed and repaired through a 7 cm incision across the mother’s uterus (womb).
Risks of open fetal surgery include an increased incidence of preterm birth, the need for a cesarean delivery, and uterine rupture.
To reduce the risks associated with a large uterine incision, in 2014 a multidisciplinary team at Texas Children’s performed an experimental fetoscopic closure of a neural tube defect – the first in the nation.
In this pioneering minimally invasive procedure, the spinal defect is repaired through two tiny (4 mm) incisions in the uterus, using a small camera known as a fetoscope.
The fetoscopic repair offers the same improved outcomes for the infant after birth as open fetal surgery, with significant additional benefits that come with using a less invasive approach, including:
As of June 2021, our fetal center physicians have completed approaching 100 fetoscopic repairs for spina bifida, more than any other fetal center in the United States. We have now closed the research aspect of this procedure at our center based on experience and consistent outcomes and now offer this procedure as a standard of care.
About the Procedure
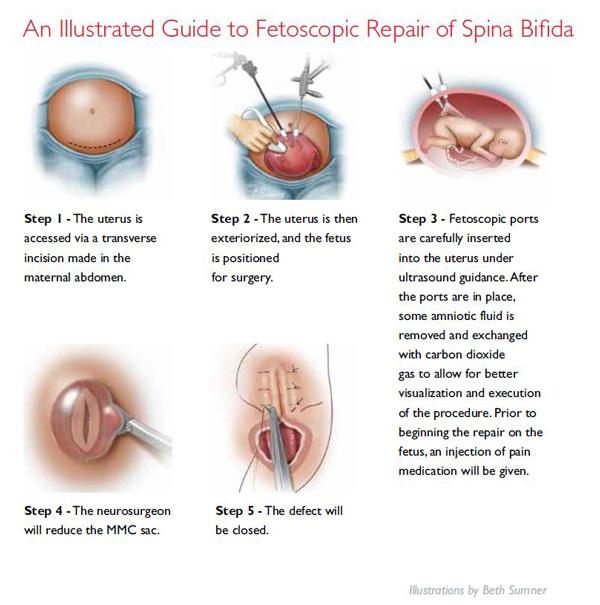
Fetoscopic repair surgery is typically performed between 19 and 26 weeks of gestation. The mother is given general anesthesia and medication to prevent contractions. The fetus receives pain medication prior to the repair.
During the procedure, the mother’s abdomen is opened to expose the uterus and the uterus is lifted out. Two 4-millimeter incisions are made in the uterus and fetoscopic ports are inserted. Some amniotic fluid is then removed and replaced with carbon dioxide gas to improve visualization.
A small scope with a camera on the end and tiny surgical instruments are inserted into the uterus through the ports. Guided by ultrasound, the surgeon closes the defect, protecting the fetal spinal column and nerves from infection and injury for the remainder of the pregnancy. The uterus is returned to the abdomen, the abdominal incision is closed and gestation resumes.
As with any surgical intervention, fetal surgery to repair spina bifida involves risks, including:
Talk with your doctor about these risks to help you and your family decide if the benefits of fetal intervention outweigh the potential complications.
Following fetal surgery, the mother will stay in the hospital 4 to 7 days. Mother and baby will be closely monitored for the remainder of the pregnancy.
Fetoscopic repair patients that meet a defined criteria of post-surgery clinical stability as well having the necessary maternal, neonatal, and neurosurgical care team and facility resources near home may be released back to their referring provider a few weeks after surgery for ongoing care until delivery. Patients that undergo open repair are generally advised and expected to remain under the care of our Fetal Center team from the time of surgery until their delivery.
A comprehensive evaluation of your pregnancy is essential to determining whether fetal surgery for myelomeningocele is an appropriate intervention. Patients who meet all inclusion criteria and none of the exclusion criteria of the MOMS trial are considered candidates for prenatal spina bifida repair.
If you and your baby are both candidates for fetal surgery, you will meet with our fetal specialists to discuss the risks and benefits of the procedure in detail, to help you and your family decide the best treatment approach for you.
Our patients are counseled on both open-hysterotomy repair and fetoscopic repair. Open hysterotomy is generally considered the clinical standard of care for prenatal repair. However, given the experience and outcomes in our Fetal Center, fetoscopic repair is also considered standard of care in our institution.
Guidelines for both fetoscopic and open procedures are based on the criteria set forth by the MOMS trial.†
Inclusion Criteria
Exclusion Criteria
†Adzick, S., Thom, E., Spong, C., Brock, J., Burrows, P., Johnson, M., Farmer, D. (2011). A randomized trial of prenatal versus postnatal repair of myelomeningocele. New England Journal of Medicine, 364, 993-1004.
We welcome all referrals. Candidates are carefully evaluated and accepted for maternal-fetal surgery on a case-by-case basis. Please contact us at 832-822-2229 if you are a physician and would like to discuss the eligibility of your patient for fetal surgery.
Medical algorithm of fetal myelomeningocele neural tube defect (Revised 9/2015)
As of January 2019, Texas Children’s Fetal Center has completed 100 prenatal neural tube defect (NTD) surgical repair procedures to treat spina bifida, more than half of which were fetoscopic in-utero repairs.
View data on our experience and outcomes treating spina bifida and neural tube defects
The Future of Healing for Neural Tube Defects: Fetoscopic Repair of Spina Bifida
Texas Children’s Fetal Center is one of the oldest and most experienced programs in the nation. We have a history of leading the development and implementation of innovative fetal therapies and procedures such as fetoscopic in-utero closure of a neural tube defect, offering families new options for the treatment of severe spina bifida and other fetal anomalies.
Here, you and your baby will receive expert maternal, fetal and pediatric care for spina bifida, all in one location. Our multidisciplinary team includes some of the nation’s top maternal-fetal medicine (MFM) specialists, fetal surgeons, pediatric neurosurgeons, fetal imaging experts, neonatologists, and pediatricians, including a renowned team of experts at Texas Children’s Spina Bifida program dedicated to the complex care of children born with spina bifida.