Topics

What are Lung Lesions?
Lung lesions are abnormal growths of lung tissue that form during fetal development. There are several different types, which we collectively call “congenital lung malformations” or “CLMs”. The most common type of lung lesion is Bronchial Atresia (BA). Another common type is Congenital Cystic Adenomatoid Malformation (CCAM).
Sometimes CLMs are referred to as Congenital Pulmonary Airway Malformations, or CPAMs, but since this term is used differently by surgeons, radiologists and pathologists and from center to center, we prefer the term CLM.
What is a Congenital Pulmonary Airway Malformation (CLM)?
A CLM is a mass of abnormal lung tissue, which may be filled with fluid or other material. These lesions vary in size and appearance with each fetus. They can also grow and change dramatically during pregnancy.
Bronchial atresia occurs when one of the small airways (a bronchus) in the fetus’s lung doesn’t develop properly and is obstructed, causing the piece of lung connected to that bronchus not to develop normally. There is overlap in the pathology of these lesions, and we believe this represents a common mechanism to their formation, with different CLM types occurring based on timing and completeness of bronchial obstruction.
While sometimes referred to as tumors, the vast majority of CLMs are benign, or not cancerous.
How does CLM affect my baby?
The impact on your baby’s health will depend on the size of the mass and its growth during pregnancy. Most babies with CLM do well, with normal fetal development and lung function. The mass may grow but not cause any problems or it may shrink making it difficult to see them late in gestation. All of these babies should be evaluated postnatally.
In about 10-15% of fetuses, the lesion may grow rapidly and become so large it compresses the lungs and pushes against the fetal heart, displacing it and other chest structures and causing the baby’s heart to work harder. This can lead to a condition known as hydrops, where fluid accumulates in different areas of the fetus’s body, and may be a sign of fetal heart failure.
How does CLM affect my pregnancy?
In rare cases, when the CLM causes serious complications to the fetus’s health, the mother may develop mirror syndrome, where the mother’s health mirrors the health of her fetus, requiring immediate delivery.
Close monitoring during pregnancy is also vital for the early detection of preeclampsia.
Types of CLMs
At Texas Children’s Fetal Center, our specialists are experienced in the diagnosis and treatment of the full spectrum of these rare fetal lung defects.
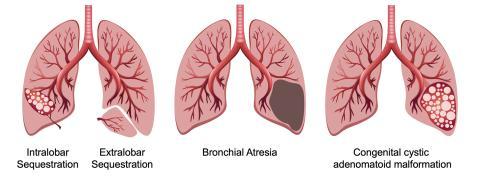
- Congenital cystic adenomatoid malformation (CCAM): A CCAM may be a large cyst, known as a macrocystic lesion, or it may be made up of many small cysts, known as a microcystic lesion;
- Bronchial atresia (BA): BA represents obstructed lung tissue and may also show cysts on imaging, due to abnormal development of the obstructed lung;
- Bronchopulmonary sequestration (BPS): BPS is identical to BA, except that there is a blood vessel that comes directly from the aorta to supply the CLM; and
- Congenital lobar overinflation (CLO): CLO is similar to BA, except that the obstructed bronchus is incomplete such that fluid can enter the obstructed lobe of lung but cannot escape, causing the lobe to become progressively more distended.
Cause and Prevalence
There is no known cause for CLMs.
The birth defect is rare, occurring in approximately 1 out of every 30,000 pregnancies. It typically isn't associated with other birth defects or genetic abnormalities.
Testing and Diagnosis
CLMs are often detected before birth during a routine ultrasound at around 18 to 20 weeks of pregnancy. The lesion may look like a solid, bright mass or it may look fluid-filled.
If CLM is diagnosed during pregnancy, you may be referred to a fetal center for a comprehensive evaluation and specialized care.
At Texas Children’s Fetal Center, we arrange for you to visit as quickly as possible to meet with a team of specialists experienced in treating fetal lung lesions, including fetal radiologists, maternal-fetal medicine physicians, surgeons and neonatologists. Our specialists will perform a comprehensive evaluation and additional testing to gain critical information about your fetus’s lung lesion and identify any other conditions.
Testing may include:
- Anatomy ultrasound to confirm the diagnosis, evaluate the lesion, exclude complications and look for other abnormalities
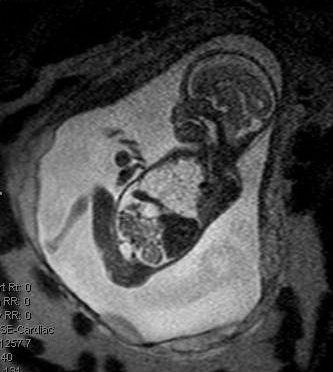
- Fetal MRI for more detailed information about the severity of your fetus’s condition, including the size and exact location of the CLM and how the lesion is affecting lung development and the surrounding chest structures
- Fetal echocardiogram to evaluate the impact of the mass on your fetus’s heart structure and function
Following this detailed assessment of the CLM, our specialists will meet with you about the results, answer any questions you have, and provide recommendations based on your fetus’s unique CLM, to help you make the most informed decisions regarding care and treatment. We are equipped to address the full spectrum of CLM conditions, with unique expertise in the most complex and challenging cases.
Treatment during Pregnancy
You and your fetus will be closely monitored throughout your pregnancy with regular ultrasounds to assess the growth of the lesion and the impact on your fetus’s health.
The frequency of your ultrasounds will depend on the size of the lesion and how it is affecting the fetus. At each ultrasound we calculate the size of the mass relative to your fetus, known as a “CLM Volume Ratio” (CVR). We use this measurement, and data gained from our experience treating fetal lung lesions, to help predict the risks to your fetus and to guide treatment decisions.
While the severity of CLM varies widely depending on specific type, size and growth, in most cases treatment isn’t required during pregnancy.
If the CLM is large and growing too quickly, the mother may be given two steroid injections to slow the growth of the fetal lung lesion and help alleviate any signs of hydrops.
In rare cases, fetuses with CLM develop complications that require urgent fetal intervention.
Fetal Intervention
If your fetus shows signs they are developing complications from the lesion, fetal therapy may be recommended. Treatment options include draining the fluid component of the lesion to reduce its size and, in life-threatening cases, open fetal surgery to remove the CLM.
Minimally Invasive Fetal Shunt. Large, fluid-filled lesions may be treated with a drainage procedure known as thoracentesis. In this minimally invasive procedure, a thin needle is placed through the mother’s uterus and into the fetal lung lesion to draw out the fluid, decreasing the size of the lesion. To prevent the fluid from building up again, a straw-like tube known as a shunt may be placed in the fetal chest, enabling fluid to continually drain from the lesion into the uterus.
Open Fetal Surgery. In rare cases, open fetal surgery to remove the lesion may be the only option for the fetus to survive. Open fetal surgery is reserved for those cases involving a large, solid lung mass that cannot be drained and, despite medical treatment, continues to compress the heart, with evidence of hydrops and a high risk of heart failure.
During open fetal surgery, the mother’s abdomen and uterus are opened and then the fetal chest, and the lung mass is removed (known as a lobectomy). Texas Children’s Fetal Center is one of the few in the world to have successfully performed this procedure for a life-threatening case of CLM.
Delivery
Typically babies with CLM can be carried until term and delivered vaginally.
In rare cases, when the fetus shows signs of complications such as hydrops, the mother may develop mirror syndrome and require immediate delivery.
For the best possible outcomes, fetuses with moderate- and large-sized CLMs should be delivered at a hospital with the expertise and resources required to treat rare CLMs, including the highest level of neonatal intensive care (NICU), if needed. Delivery and postnatal care should be carefully planned and coordinated with a team of maternal-fetal medicine specialists, neonatologists, anesthesiologists, cardiologists, and surgeons experienced in the EXIT (ex-utero intrapartum treatment) procedure, to address potential breathing issues at birth.
Our specialists comprise the Texas Children’s Congenital Lung Lesion program to coordinate your baby’s care across an expert, multidisciplinary team, ensuring the best possible care from prenatal diagnosis to birth, and continuing throughout childhood and adolescence.
Surgery during Delivery – EXIT-to-Resection Procedure
If your fetus’s lung lesion is very large and stays large until the time of delivery, it can cause breathing difficulties at birth. Your doctor may recommend a cesarean delivery with a fetal surgery performed at delivery known as an “EXIT (ex-utero intrapartum treatment)-to-resection” procedure. This approach enables removal or “resection” of the lung lesion while your baby is still connected to the placenta via the umbilical cord, ensuring the newborn isn’t deprived of oxygen at birth.
In an EXIT procedure, the mother’s abdomen and uterus are opened, as in a C-section, and the baby’s head and part of the upper body are delivered. While the baby is still attached via the umbilical cord, and receiving oxygen from the mother, the surgeon removes the lung lesion to improve breathing after delivery. When the baby is stable enough, it is fully delivered and the umbilical cord is cut.
Following an EXIT procedure, your baby will be taken to a neonatal intensive care unit (NICU) for observation and care. In some cases the baby may need to be placed on ECMO (extracorporeal membrane oxygenation), a heart-lung bypass machine that performs the work of the heart and lungs while the newborn recovers.
Surgery for Newborns with CLM
In some cases, treatment for CLM will involve surgery after birth to remove the lesion. Removal of the lesion is recommended to prevent the development of infection or possible cancer later in life.
The timing of the surgery will depend on the health of your baby at birth.
If your newborn experiences breathing difficulties or a prolonged need for oxygen after delivery, surgery to remove the lesion may be recommended before going home.
Babies with no problems at birth are typically able to go home with the mother. A consultation with a pediatric surgeon and a follow-up appointment at two months of age is recommended to discuss management and removal of the lesion, if needed. Surgery is generally recommended between two and six months of age to take advantage of the growth potential of the remainder of the lungs.
Long-Term Outcomes
Most fetal lung lesions can be successfully treated and most fetuses with these conditions do very well. Even those with severe cases may have a good prognosis with early detection, close monitoring and timely treatment.
At Texas Children’s Congenital Lung Lesion Program, our specialists will follow your child from their fetal diagnosis to adulthood, for the best possible pulmonary health and neurodevelopmental outcomes.
Why Texas Children’s Fetal Center?
- A single location for expert maternal, fetal and pediatric care. At Texas Children’s Hospital, you and your fetus can get the specialized care required for the diagnosis and treatment of fetal lung lesions all in one location, for highly coordinated care and treatment planning. If needed, Texas Children’s Hospital is home to the first neonatal intensive care unit (NICU) to be designated by the Texas Department of State Health Services (DSHS) as a level IV NICU, the highest level of care available for premature and critically ill newborns.
- A skilled, experienced team with proven outcomes. We have a dedicated team of maternal-fetal medicine specialists, surgeons, neonatologists, radiologists, cardiologists, ECMO specialists, anesthesiologists and others who work in concert to care for you and your baby every step of the way. With their combined expertise and unified approach, these physicians offer the best possible care for fetuses with CLMs.
- We care for your child’s needs at every stage of life. Our comprehensive approach starts with your first prenatal visit for CLM and continues through your child’s delivery, postnatal care, childhood and into adulthood, thanks to one of the nation’s leading teams of fetal and pediatric specialists for the treatment of rare birth defects.
Patient Stories
Fetal Imaging and Congenital Cystic Adenomatoid Malformation: Becky's Story
Volumes & Outcomes
View data on our experience and outcomes treating fetal lung lesions
For more information or to schedule an appointment, call Texas Children’s Fetal Center at 832-822-2229 or 1-877-FetalRx (338-2579) toll-free. Our phones are answered 24/7. Immediate appointments are often available.