Topics
A lower urinary tract obstruction (LUTO) is a rare birth defect in which the fetus has a blockage in the urethra, the tube that carries urine out of the baby’s bladder and into the amniotic sac.
LUTO is also known as bladder outlet obstruction.
How does LUTO affect my baby?
An obstruction in the lower urinary tract can cause serious complications, including:
- Bladder damage. With no way out, the fetal urine overfills the bladder causing it to become enlarged, damaging this thin-walled structure.
- Kidney damage and kidney failure. The backup of urine puts pressure on the fetal kidneys. This can cause progressive, permanent damage and the risk of kidney failure.
- A lack of amniotic fluid. Fetal urine is the main component of amniotic fluid. When the flow of urine is blocked, the fluid in the amniotic sac can significantly decrease or disappear. This is called oligohydramnios (too low) or anhydramnios (no fluid).
- Underdeveloped lungs and breathing difficulties at birth. The fetus breathes amniotic fluid in and out to help the lungs develop properly. Without adequate fluid, the baby’s lungs may be too small (pulmonary hypoplasia) at birth to support their oxygen needs.
- Deformities of the face and extremities. Known as Potter sequence, these malformations are caused by a lack of amniotic fluid.
Cause and Prevalence
LUTO is rare, occurring in an estimated 2.2 of every 10,000 births. The cause of the birth defect is unknown, but genetics may play a role in some cases.
LUTO is more common in males. For example, males are four to five times more likely to develop a less severe form of LUTO known as hydronephrosis, where there is an obstruction in the ureter tube that connects the kidney and bladder.
Types of LUTO
There are several types of lower urinary tract obstructions, including:
- Posterior urethral valves, where a thin piece of tissue blocks the urethra
- Urethral atresia, where the urethra is missing or completely closed, so there is no outlet from the bladder to the amniotic sac
- Urethral stenosis, where the urethra is so narrow the urine can’t flow out in large enough volumes
Testing and Diagnosis
LUTO is typically diagnosed late in the first trimester or early in the second trimester through routine ultrasound. The imaging may reveal an enlarged fetal bladder, swelling of the kidneys, and a low amount of amniotic fluid. On ultrasound, the enlarged bladder and a dilated urethra may resemble a keyhole, known as a “keyhole sign” of LUTO.
If LUTO is diagnosed or suspected, you may be referred to a fetal center for a comprehensive evaluation and specialized care.
At Texas Children’s Fetal Center, we arrange for you to visit as quickly as possible to meet with a team of specialists experienced in diagnosing and treating this rare birth defect, including maternal-fetal medicine (MFM) physicians, fetal surgeons, fetal imaging experts, genetic counselors, neonatologists, pediatric nephrologists and pediatric urologists.
Testing at our center may include:
- Anatomy ultrasound to confirm the diagnosis, evaluate the obstruction, and look for other abnormalities
- Fetal MRI for more detailed information about the severity of your baby’s condition
- Fetal echocardiogram to evaluate your baby’s heart
- Amniocentesis and chromosomal analysis to screen for genetic abnormalities
- Fetal bladder tap (vesicocentesis) to obtain a urine sample and evaluate your baby’s kidney function
Following this detailed assessment, our specialists will meet with you about the results, provide treatment recommendations based on your baby’s unique condition, and counsel you about the potential risks and benefits, to help your family make the most informed decisions.
Through comprehensive, highly personalized treatment plans, Texas Children’s has some of the best LUTO outcomes in the United States. Today many institutions are adopting our proposed criteria for treatment selection.
Treatment During Pregnancy
Treatment for LUTO depends on the severity of the condition and the impact on fetal kidney function. Mild cases may have little or no effect on the fetus or baby and require only close observation, with no treatment necessary. Moderately serious cases may require surgery after birth to repair an obstruction or reflux (backward flow of urine).
In some cases of severe obstruction, where there is evidence of preserved kidney function, fetal intervention may be an option.
Potential interventions during pregnancy include:
- Repeat fetal bladder drain, known as vesicocentesis (uncommon)
- Fetal vesicoamniotic shunt placement
Fetal Shunt Placement
The most common fetal intervention for LUTO is a shunt or draining tube placed in the fetal bladder during pregnancy. One end of the tube is inserted in the bladder and the other end is left outside of the baby’s stomach. The hollow tube allows the urine to drain out of the fetal bladder and into the amniotic sac.
The goal is to restore and maintain a normal fluid level in the amniotic sac for proper fetal lung development, improving the baby’s chance of survival after birth. The shunt may also reduce the pressure inside the fetal bladder and kidneys, however it may not prevent further kidney damage.
Our team will review the risks to you and your baby and carefully weigh the potential risks and benefits before proceeding with fetal intervention.
About the Procedure
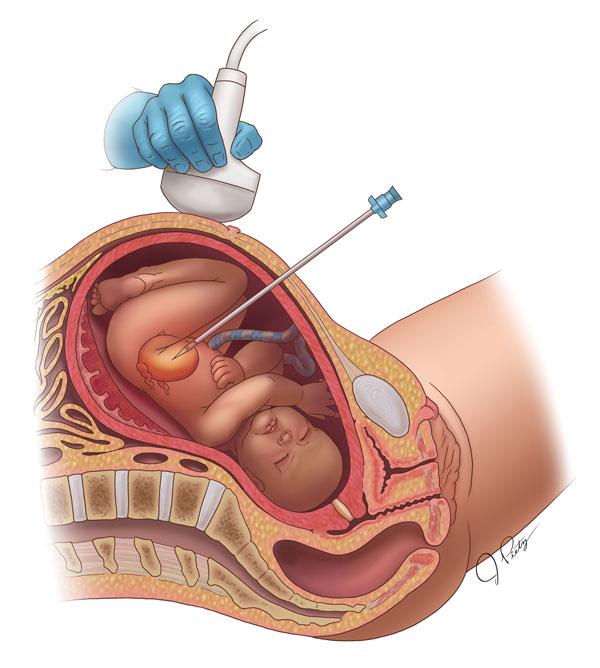
The fetal shunt procedure is performed in the hospital on an inpatient basis. The mother is given IV sedation, which also sedates the fetus, as well as antibiotics and local anesthesia. The fetus will also receive an injection to temporarily paralyze it during the procedure and for pain management.
During the minimally invasive procedure, ultrasound guidance is used to insert a needle through the mother’s abdomen and uterus and place the shunt in the fetal bladder. Fluid may also need to be added to the amniotic sac during the procedure.
The shunt will remain in the bladder until the baby is born. Mother and baby will be closely monitored throughout the remainder of the pregnancy.

Is my baby a candidate for fetal intervention?
LUTO requires highly individualized treatment tailored to the unique needs and condition of each mother and baby. An extensive prenatal evaluation is critical to determining if your baby may benefit from fetal intervention.
Our fetal center continues to gather data on LUTO patients to establish standards for evaluating which treatments are most successful based on the severity of the condition. These standards look at:
- The chemistry of fetal urine, to evaluate kidney function
- Ultrasound evidence of kidney function
- Amniotic fluid levels
- Chromosome analysis
Delivery
Babies with LUTO should be delivered at a hospital equipped with the resources required to treat these rare birth defects, including a neonatal intensive care unit (NICU) and breathing support for newborns with underdeveloped lungs.
Delivery and postnatal care should be carefully planned and coordinated with a multidisciplinary team experienced in working together to optimize LUTO outcomes.
Our fetal center specialists work closely with Texas Children’s neonatologists, pediatric nephrologists and pediatric urologists, among many others, to coordinate your baby’s care from prenatal diagnosis to birth to postnatal care.
LUTO typically does not impact the decision to have a vaginal or cesarean delivery.
Treatment After Birth
After birth, Texas Children’s pediatric nephrologists and urologists will conduct additional tests to analyze your baby’s kidney and bladder function and determine the cause and impact of the defect.
Some babies may need to stay in the neonatal intensive care unit for weeks or months, depending on lung function and the severity of kidney damage.
In some cases, babies will need a surgery to correct how urine leaves the body (vesicostomy). This is not always permanent. Additional surgery and ongoing renal replacement therapy, such as dialysis or kidney transplant, may be necessary if kidney failure occurs.
Why Texas Children’s Fetal Center?
- A single location for expert maternal, fetal and pediatric care. At Texas Children’s Hospital, you and your baby can get the specialized care required for the diagnosis and treatment of LUTO all in one location, avoiding the need to transport your critically ill newborn. Texas Children’s Hospital is home to the first neonatal intensive care unit (NICU) to be designated by the Texas Department of State Health Services (DSHS) as a level IV NICU, the highest level of care available for premature and critically ill newborns.
- A skilled, experienced team with proven outcomes. We have a dedicated team of maternal-fetal medicine specialists, surgeons, neonatologists, fetal imaging experts, pediatric nephrologists, pediatric urologists, and others who work in concert to care for you and your baby every step of the way, using proven protocols we’ve developed over the years. With their combined expertise and unified approach, this remarkable team offers the best possible care for babies with LUTO.
- We care for your child’s needs at every stage of life. Our comprehensive approach starts with your first prenatal visit for LUTO and continues throughout your child’s delivery, postnatal care, and childhood, as needed, thanks to one of the nation’s leading teams of fetal and pediatrics specialists for the treatment of rare birth defects.
Patient Videos
- Luke's Story: Fetal intervention for Lower Urinary Tract Obstruction
- Eli’s Story: Fetal intervention for LUTO
Research & Clinical Trials
- Fetal lower urinary tract obstruction: proposal for standardized multidisciplinary prenatal management based on disease severity
- Defining and predicting 'intrauterine fetal renal failure' in congenital lower urinary tract obstruction
Additional Information and Resources
- Medical algorithm for LUTO
- Nephrology - Kidney (Renal) Program
- Texas Children's Hospital - Urology Program
Patient Stories

Extraordinary Outcome for Devastating LUTO Case
Before Luke Vela was even born, his big brother nicknamed him Tuff because of the challenges he’d already overcome.

Eli's story: Traveling to Texas for a lifesaving fetal surgery
On Oct. 31, baby Eli will be five months old, but his journey getting here was nothing short of a miracle. It all started during Lacey Prejean's 12-week pregnancy appointment.
For more information or to schedule an appointment,
call Texas Children’s Fetal Center at 832-822-2229 or 1-877-FetalRx (338-2579) toll-free.
Our phones are answered 24/7. Immediate appointments are often available.