Topics
Chorioangioma is a tumor of the placenta. The placenta is the organ that develops in the uterus during pregnancy and attaches to the uterine wall, nourishing the growing fetus via the umbilical cord.
Chorioangiomas are vascular tumors, meaning they are made up of blood vessels. In the majority of cases the tumor is benign (noncancerous).
Small chorioangiomas typically cause no symptoms and complications. If the chorioangioma is large, measuring more than 4 cm, in some cases it can pose serious risks to the pregnancy and the fetus, including fetal heart failure.
Cause
The cause of chorioangioma is unknown. The abnormal masses form in the chorionic tissue, the tissue on the fetal side of the placenta.
Chorioangiomas occur in an estimated 1% of pregnancies. The tumors are seen more often in pregnancies where the fetus is female and in those involving multiples (twins, triplets, etc.).
How does chorioangioma affect my baby?
A large chorioangioma can cause serious fetal and maternal complications.
In some cases, the blood vessels in a large chorioangioma may cause rapid “shunting” of blood to the tumor. The increased volume of blood flow (known as high cardiac output) forces the fetal heart to work harder, potentially causing it to enlarge and weaken. Over time, heart failure may occur.
Risks to the fetus include:
- Anemia (lack of red blood cells)
- Thrombocytopenia (inability to clot due to lack of platelets)
- Non-immune hydrops (fluid buildup and swelling in multiple areas of the baby’s body)
- Enlargement of the heart (cardiomegaly)
- Fetal heart failure
- Intrauterine growth restriction, caused by a mass protruding into the amniotic cavity)
- Fetal stroke
- Umbilical vein thrombosis (clot in umbilical cord vein)
- Neonatal death due to heart failure
Potential maternal complications include:
- Polyhydramnios, a build-up of amniotic fluid in the womb
- Premature delivery
- Preeclampsia (high-blood pressure with signs of organ damage)
- Placental abruption (placenta detaches from the uterus before delivery, causing bleeding)
- Malpresentation (baby abnormally positioned at delivery)
- Need for a cesarean delivery
- Maternal mirror syndrome (fluid retention and swelling, mirroring the health of the fetus)
- Postpartum hemorrhage
Diagnosis
Larger chorioangiomas may be diagnosed during a routine prenatal ultrasound, often in the second trimester.
Small chorioangiomas that are not causing symptoms often go undetected. In some cases, a small chorioangioma isn’t discovered until after birth, when the placenta is expelled and evaluated.
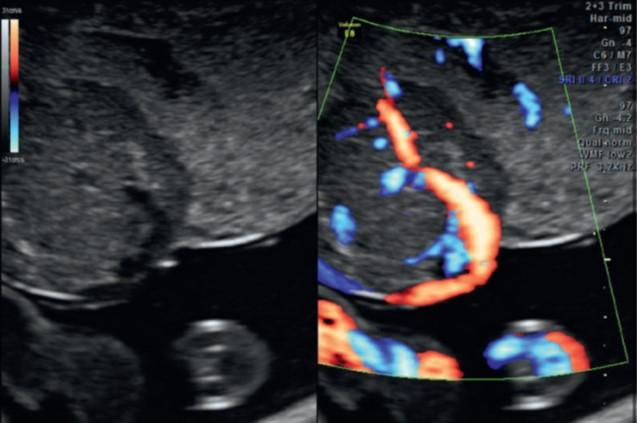
Accurate diagnosis is important to differentiate chorioangioma from other placental abnormalities. On imaging, chorioangioma appears as a solid mass with a clearly defined contour, or outline. The mass is usually located near the umbilical cord “insertion site” (where the umbilical cord attaches to the placenta). The tumor may protrude into the amniotic cavity.
A diagnosis during pregnancy ensures mother and fetus are closely monitored for proper treatment and timely delivery, optimizing outcomes.
Specialized Evaluation and Prenatal Care
If a chorioangioma is diagnosed or suspected during pregnancy, you may be referred to a fetal center for further evaluation.
At Texas Children’s Fetal Center, we arrange for you to visit as quickly as possible for a comprehensive assessment by a team of specialists experienced in the diagnosis and treatment of placental tumors, including maternal-fetal medicine physicians (OB/GYNs specializing in high-risk pregnancies), fetal imaging experts, fetal cardiologists, and neonatologists.
Additional testing will be performed using state-of-the-art imaging technologies and techniques that provide detailed views of your baby’s condition, for the most accurate diagnosis and treatment planning. Testing may include:
- High-resolution anatomy ultrasound to confirm the diagnosis and look for other abnormalities
- Ultra-fast MRI for a more detailed view of fetal anatomy
- Fetal echocardiogram to evaluate the baby’s heart
- Doppler ultrasound to examine blood flow to the tumor
- Amniocentesis and chromosomal analysis to identify any chromosomal anomalies
Our specialists will then meet with you about the results, discuss treatment recommendations and answer any questions your family has, to help you make the most informed decisions regarding your baby’s care and treatment.
Treatment During Pregnancy
Mother and baby will be closely monitored throughout pregnancy with frequent ultrasounds and fetal echocardiograms to assess the growth of the tumor, amniotic fluid level, fetal heart function, and fetal growth, among other factors, for early detection of complications.
In some cases, fetal intervention may be recommended. Treatment strategies during pregnancy may include:
- Steroids to accelerate fetal lung maturity if early delivery becomes necessary
- Amnioreduction, a procedure used to reduce the amniotic fluid level, decreasing the risk of preterm labor (similar to an amniocentesis)
- Fetal blood transfusions to treat anemia
- In fetuses at risk of heart failure, treatment to stop or reduce the blood supply to the tumor, such as fetoscopic or interstitial laser ablation (using laser energy to seal blood vessels)
Talk with your healthcare team about the potential benefits and risks of invasive fetal therapies, to help you make the best decision for your family.
Delivery
We recommend delivery at a hospital with the expertise and resources required to care for pregnancies involving chorioangioma, including the highest level neonatal intensive care unit (NICU). Early delivery may be required if complications occur.
Delivery and postnatal care should be carefully planned and coordinated by a team of maternal-fetal medicine physicians, neonatologists, and pediatric specialists experienced in working together to treat these rare placenta abnormalities.
Our Fetal Center team works closely with pediatric experts from Texas Children’s Hospital, consistently ranked one of the best children’s hospitals in the nation by U.S. News & World Report. For our patients, that means seamless access to the critical care services and specialists your baby may need after birth, with no transfers required. It also means the pediatric experts responsible for treating your child have been part of their care team prior to birth.
Treatment After Birth
Treatment after birth depends on the newborn’s symptoms and overall health.
Some babies may be born with complications that include severe thrombocytopenia (clotting disorder) and anemia, requiring platelet and blood transfusions, or the baby may require treatment for non-immune hydrops, including the removal of excess fluid and breathing support.
Expert examination of the placenta is important after birth to confirm the diagnosis of a chorioangioma and that the tumor was benign.
Postnatal Care Team
Depending on your baby’s condition, his or her postnatal care team may include:
- Neonatologist
- Pediatric cardiologist
- Hematologist
- Primary pediatrician
Why Texas Children’s Fetal Center?
- A single location for expert maternal, fetal, and pediatric care. At Texas Children’s Hospital, mother and baby receive the specialized care required for the diagnosis and treatment of chorioangioma all in one location, for highly coordinated care and treatment planning, including immediate access to our level IV NICU if needed.
- A skilled, experienced team with proven outcomes. We have a dedicated team of maternal-fetal medicine specialists, fetal imaging experts, neonatologists, pediatric cardiologists, pediatric hematologists and others who work in concert to care for you and your baby every step of the way, using proven protocols we’ve developed over the years. With their combined expertise and unified approach, this team offers the best possible care for pregnancies involving placental tumors.
- We care for your child’s needs at every stage of life. Our comprehensive approach starts with your first prenatal visit and continues through delivery, postnatal care, and childhood, as needed, thanks to one of the nation’s leading teams of fetal and pediatric specialists for the care and treatment of rare fetal conditions.
Videos
Additional Resources
For more information or to schedule an appointment,
call Texas Children’s Fetal Center at 832-822-2229 or 1-877-FetalRx (338-2579) toll-free.
Our phones are answered 24/7. Immediate appointments are often available.